One in Four Americans report to having suffered a concussion, but not nearly that amount know what to do about it.
The Silent Epidemic
There is a grave misconception of what a mild traumatic brain injury (MTBI) truly is among our general population. This may be due to the lack of education about them, and is likely conjugated with how much of a red herring the fallout and symptoms of a concussion can be for the affected person.
The NFL has recently brought some light to the issue. The New York Times reported that of 111 studied NFL players, 110 of them showed signs of chronic traumatic encephalopathy, which is a degenerative brain disease that is caused from multiple instances of blunt trauma.
Between 2001 and 2009, an estimated 173,285 people under age 19 were treated in hospital emergency rooms for MTBI according to the CDC. These were caused by sports and recreational activities. The University of Pittsburgh estimates that there are over 300,000 cases treated every year just related to sports. That’s nearly 1% of the US population annually.
What’s not being reported are construction accidents, bathroom slips, and the common “boys will be boys” sort of incidents.
1 in 4 Americans report to having had a concussion in their lives. This is something that affects more people than heart disease or cancer. So why don’t we see donation programs and ribbons in support of this ailment? I think because the information about it’s long-term damages just isn’t widespread. There is a mountain of literature on just how dangerous these brain injuries can be. So much that I couldn’t possibly give an overview fully in an intro section.
But what I can do is help you recognize and treat them. So here goes.
Mechanism of Injury
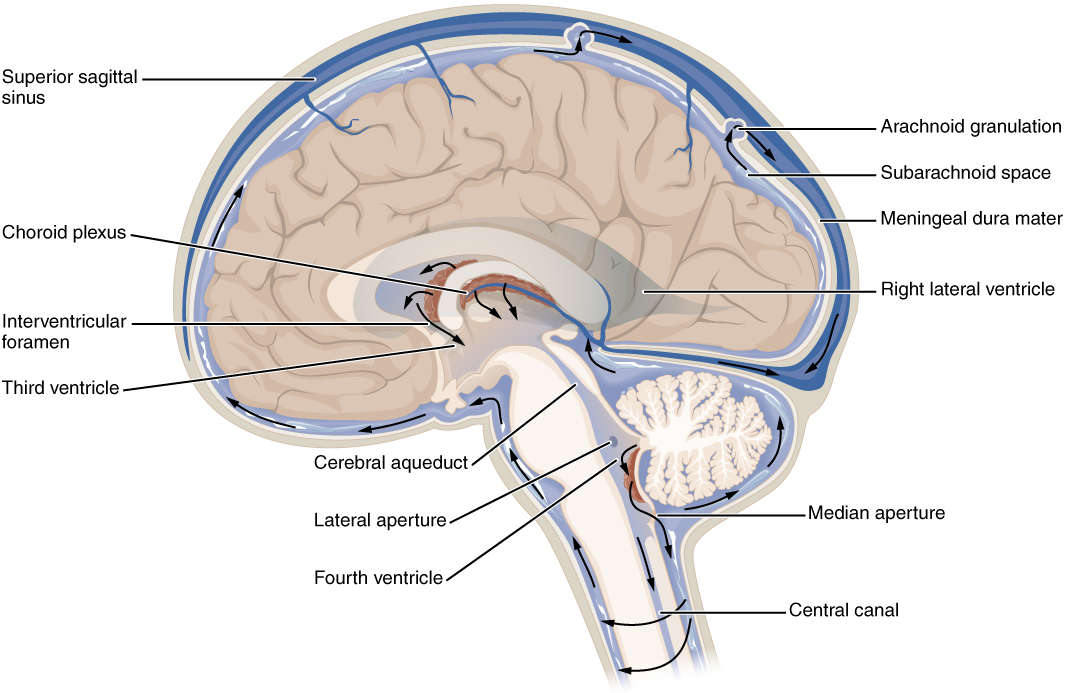
The brain floats, if you weren’t aware.
Your skull is a large pickle jar that the brain is nestled into by a cushioning layer of liquid comprised of Cerebral Spinal Fluid. Your brain matter is not meant to make contact with your skull and avoids this by remaining neutrally buoyant inside that bone melon-case you’ve got.
When a force is applied to the head of sufficient nature, the head will move. Because the brain floats, the brain will not. This will cause your moving skull to impact your stationary brain. As we had just said, brain matter is not meant to make contact with your skulls.
Brain matter is incredibly hydrated, and as a result very soft and vulnerable to edema and hemorrhage. When you see dark spots on a CT scan from a patient with a brain injury, you’re usually looking at blood inside the brain cavity. Obviously, this is bad.
This tissue can recover at different paces and to different degrees depending on the person and nature of the injury, as well as number of previous concussions. The more you get, the harder they are to recover from. If you can even recover fully at all.
SYMPTOMS
Mild
Mild doesn’t mean it’s not worth worrying about. Just like a leaky faucet can still eventually fill a bath tub, continuous mild trauma to the brain can stack up to very permanent and debilitating losses of function. These are the most commonly unreported types of brain injuries. If you know someone took a fall or got hit on the noggin, be on the lookout for these symptoms.
- Headache
- Ringing in the ears
- Nausea
- Vomiting
- Fatigue or drowsiness
- Blurry vision
Severe
Severe symptoms can be tricky, as they may not present for some time after the injury. However, some of the more immediate signs that something seriously wrong are obvious and we may all know from common sense already. Items like these include:
- Pain: Constant or recurring headache
- Motor dysfunction: Inability to control or coordinate motor functions or disturbance to balance
- Sensory: Changes in ability to hear, taste or see; dizziness; hypersensitivity to light or sound
- Cognitive: Shortened attention span; easily distracted; overstimulated by environment; difficulty staying focused on a task, following directions or understanding information; feeling of disorientation, confusion and other neuropsychological deficiencies
- Speech: Difficulty finding the “right” word; difficulty expressing words or thoughts; dysarthric speech.

A useful tool to determining just how bad a concussion has gotten is to employ the Glasgow Coma Scale. This is a numerical scale that is used by medical professionals to communicate the loss of cognition that their patients have suffered.
To use it, you break down responses into sensory, verbal, and motor responses.
For eye response, you look at the eye motion of your patient. Open spontaneously is the best result, this would mean the patient is looking around naturally with no sluggish motion or loss of attention. Open to verbal command doesn’t mean the eyes only open to verbal command, but can also indicate that your patient is only able to follow whatever is making noise at that time. Open to pain means eye movement is only associated as a response to some painful stimulus. No eye opening is self explanatory.
Verbal responses are how the patient reacts to being spoken to in their own words. Ask them questions such as “What day of the week is it?” or “Who was our last Vice President?” Quick, clear, and correct answers will score as Oriented. Those who can speak relatively clearly but cannot give correct answers that they otherwise should are Confused. Mumbling completely unrelated sentences is Inappropriate Words. Incomprehensible Sounds and No Verbal Response need no explanations.
Obeys Commands is easy to understand for Motor Response. Localising Pain means that they are guarding, or actively covering or pointing to the source of their pain. Withdrawl from pain means they will try to retreat from whatever may stimulate the pain. Flexion refers to abnormal movements of limbs when the pain is stimulated, such as abduction of the arms or pronating the wrists. Extension to pain includes purely extrasensory reactions such as decerebate posture. No motor response is to be a ragdoll.
The commonly considered scale is:
Mild 13-15 GCS
Moderate 9-12 GCS
Severe <8 GCS
This can be useful to us, even if we aren’t medical professionals, because we can use their language to explain the problem. If you can let the dispatcher know that your buddy suffered a fall and hit his head and that his GCS is a 9, that dispatcher can relay that information as pertinent and possibly prioritize your transport over another mild emergency in the area.
Treatment
There’s no true replacement for taking someone to the Emergency Room. MTBI’s aren’t something that someone should just “walk off.” After getting rid of the initial fogginess, there will be processes happening in the brain that may be hindered by continuing even just your daily activities. If you have any doubt whatsoever, please refer to the professionals.
However, this is ISG. We develop our medical skills for when there is no help coming and there is no doctor. If you or a team member suffers an MTBI, what measures can we take to aid in the recovery? This can depend on a few different things, such as the severity of the injury itself.
First, we need to understand that the recovery period lasts longer than the symptoms. The brain isn’t the fastest thing to heal and that can be hindered further by wanting to go back to performing normal tasks earlier than one should. Symptoms that last only one day can often take 6-10 to fully recover from. Most of the audience here are doers and self starters. Holding yourself back from activity despite feeling ready for it will be a huge challenge.
Second, know what to avoid. We don’t want to overload your brain or take on any unnecessary cognition. These activites include
- Texting/spending time looking at your smartphone screen.
- Reading.
- Watching television.
- Playing video games.
- Listening to loud music.
- Doing any physical activity.
These are all quite stimulating to your cognitive functions. That stimulation slows or interferes with the healing process. The best medicine here is rest. Directly after the event try and find a dim, quiet place for the patient to lie down or sit in. Remove external factors that may cause irritation by trying to control the temperature and assuring them that whatever situation you were handling will be find without them for now.
MYTHS
While we’re here, let’s take the time to dispel some misconceptions.
MYTH: Concussions happen when someone is hit in the head.
FACT: A concussion can result from any rapid movement of the head, such as a car accident.
MYTH: You must lose consciousness for there to have been a concussion
FACT: Anytime one receives blunt trauma or rapid movement to the head a concussion can occur. Not just when they go unconscious.
MYTH: Don’t let someone with a concussion fall asleep, they may not wake up!
FACT: A person can go to sleep following a concussion if he or she is awake and able to hold a conversation. Sleep actually helps cure concussions. The reason why someone with a severe injury is kept awake is so that medical professionals can track the loss or gain of cognition over time to understand the severity of the injury.
MYTH: If you don’t have symptoms, you don’t have a concussion
FACT: It can take as much as 24-48 hours for symptoms to show.
MYTH: If you feel okay, you are okay
FACT: As we covered, symptoms can be delayed, and often disappear before the healing is fully finished.

Operational Concerns
There are things to consider about a patient with a concussion if they are part of a civil response team or member of your neighborhood during a Type II or III event. We know that recovery can often be lengthy, but during that time behaviors may arise as part of the concussion that seem separate but are not. This is a deep, deep subject, and highly personal to your situation. For that reason, I’ll only touch on the concepts and you can apply as needed.
Restricted Physical Activity: You may need to plan around being a pair of hands down for a while so that they may recover. This could mean having to reschedule watch shifts, or make do doing a job with less people than you previously planned for.
Irritability: People recovering from concussions are quick to anger and can react irrationally. If it’s bad, they may need items like firearms taken away from them until they’ve had time to heal. This can also cause emotional turmoil among the team if they’re not aware. Remember that they’re recovering, and hurtful things said in that context are to be taken with a grain of salt.
Environment: The healing process requires rest, relative quiet, and relative inactivity. If you’re trying to cover some ground, recognize that it may be necessary to be stationary for a day or two until the patient is in a better place to start putting some paces back on. Likewise, if you normally play lots of music for morale, it may be time to learn to enjoy some quiet moments.
Eagerness: A patient is going to be eager to recontinue duties before they’re ready as they’ll likely feel much better before they’re fully healed. You’ll have to help remind them and other members of your team that concussions are a gremlin that continues to work even after you’ve stopped feeling the effects.
Conclusion
Just because they’re common doesn’t mean they’re not serious. Our current world is full of riots where bottles, bricks, and rubber bullets are being flung through the airspace. Building damage that can cause faulty infrastructure is now abound. And during all this, things like falls and car accidents certainly aren’t getting less common. Understand the type of event an MTBI truly is and take measures accordingly. Not allowing proper recovery can have permanent cognitive effects.
It’s better to be inactive for a week than a little more stupid forever.
Play the long game, recover in the short term so you can have the mental endurance needed for the rest of your life. Thank you, and good luck.








